Covid-19’s second wave hits Sudan harder and faster
11 December 2020
While people celebrated the New Year in Khartoum recently, Khartoum’s State Ministry of Health recorded 134 new cases of the Covid-19 pandemic and seven deaths, according to the state director, Mahjoub Taj el-Sir. The state’s infection rate is a worrying trend, the director says since Khartoum State –like the rest of the country– is still woefully ill-prepared to contend with a second wave of the virus.
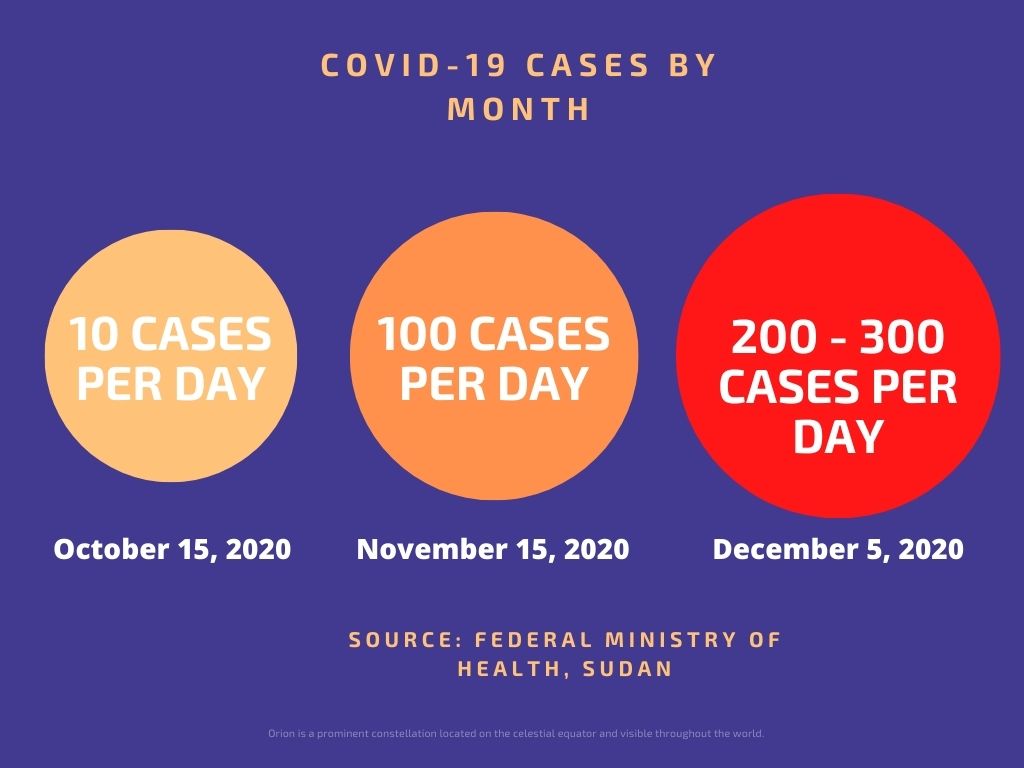 The second wave of the coronavirus has hit Sudan twice as fast with about the same number of cases and deaths reported in almost half the time of the first wave, according to the Federal Ministry of Health data. During the first two weeks of October last year, the average daily number of cases reported was less than 10 but increased to over 100 cases every day by mid-November and reached 200-300 cases daily by early December.
The second wave of the coronavirus has hit Sudan twice as fast with about the same number of cases and deaths reported in almost half the time of the first wave, according to the Federal Ministry of Health data. During the first two weeks of October last year, the average daily number of cases reported was less than 10 but increased to over 100 cases every day by mid-November and reached 200-300 cases daily by early December.
According to Taj el-Sir, the high infection rates require “the sounding of the alarm” where the capital struggles with the highest infection rates across the state. By 23 December last year, Sudan’s Central Doctors Committee reported over 35 physicians had died during the second wave of the pandemic, calling it “a heavy loss for the entire medical field in the country.”
Sudan’s central government appears pre-occupied with a myriad of other challenges, not least skyrocketing inflation and fuel prices amidst power cuts and mounting insecurity in the Darfur region, despite the gravity of the health crisis. “We hear the second wave is more dangerous than the first and we hear news of deaths every day,” says Khartoum resident Hadia Zaroug, “but we do not see the ministry’s work as it was in the days of the previous administration.” According to Zaroug, government interaction is very weak and there are no educational campaigns in neighbourhoods and public areas as there were before. “We are trying hard to isolate and protect ourselves without any support from any party.”

Cheaper medicine
But government efforts are being made. Last month, Finance Minister Hiba Mohamed said they would finance a “comprehensive plan to ward off the effects of the pandemic with a budget of 4.8 Billion Sudanese Pounds (US$ 1.3 million) within four months. Health Minister Osama Abdelrahim said in a statement last month that Sudan will use some of these funds to subsidise medicines by 60%, the largest financial support the government has provided in history. The minister also met officials from the World Health Organisation (WHO) on 20 December who received a European Union grant of 11.5 million Euros to counter Covid-19 in Sudan.
Whether these funds will be sufficient is another matter – especially considering that official Covid-19 infection rates may only be the tip of the iceberg. A study by the Imperial College of London claims only 2% of Covid-19 related deaths have been reported in Khartoum, with as many as 16,090 deaths potentially missed as of 20 November. Doctors have told Ayin that they suspect the pandemic has spread for more widely, not only in the capital but the entire country, than officially reported. In November, the Sudanese Professionals Association (SPA), the civil society body the spearheaded the revolution, labelled Covid-19 a national security threat. “The new cases announced by the ministry in its regular reports do not reflect the real epidemiological situation,” the association’s 22 November statement said. “The cases registered in private laboratories are not included in the official figures, while the government has no plans to correct this.”
The poor monitoring of Covid-19 cases is also linked to the fact that the country does not have an operating intervention plan, says Khartoum-based doctor, Bandar Noory. “This is because they [Ministry of Health] do not have an active care-access program that is supposed to operate on several fronts, such as contact tracing,” he said. Many of Khartoum’s positive cases emanate from travellers coming from the United Arab Emirates (UAE) and Saudi Arabia, Noory told Ayin, who are not properly tracked after leaving the airport. “There are also no empty beds in the isolation centres, which made patients wander around between hospitals, worsening and possibly spreading their condition –prompting some to buy oxygen tanks and just isolate at home.” Doctor Noory says private facilities are the most active in treating corona patients due to the lack of equipment and preparedness by public facilities. But the private hospitals charge prohibitively expensive services to treat the virus, Noory said, ranging from 200,000 Sudanese Pounds (roughly US$ 750) – over a year’s salary for a government doctor working in Khartoum.
With limited public health support and prohibitively expensive private care, many Khartoum residents have resorted to home care and local solutions. During this second wave of Covid-19, Nazim Khalil, a civil engineer working for the University of Khartoum, got infected. After testing positive, he received no follow up, isolated himself within his home and performed self-treatment, using vitamins, headache tablets and some local medicinal herbs suggested by neighbours. “I had no other option,” Khalil told Ayin, “there simply was no support available.”

“Dangerous and liable to explode”
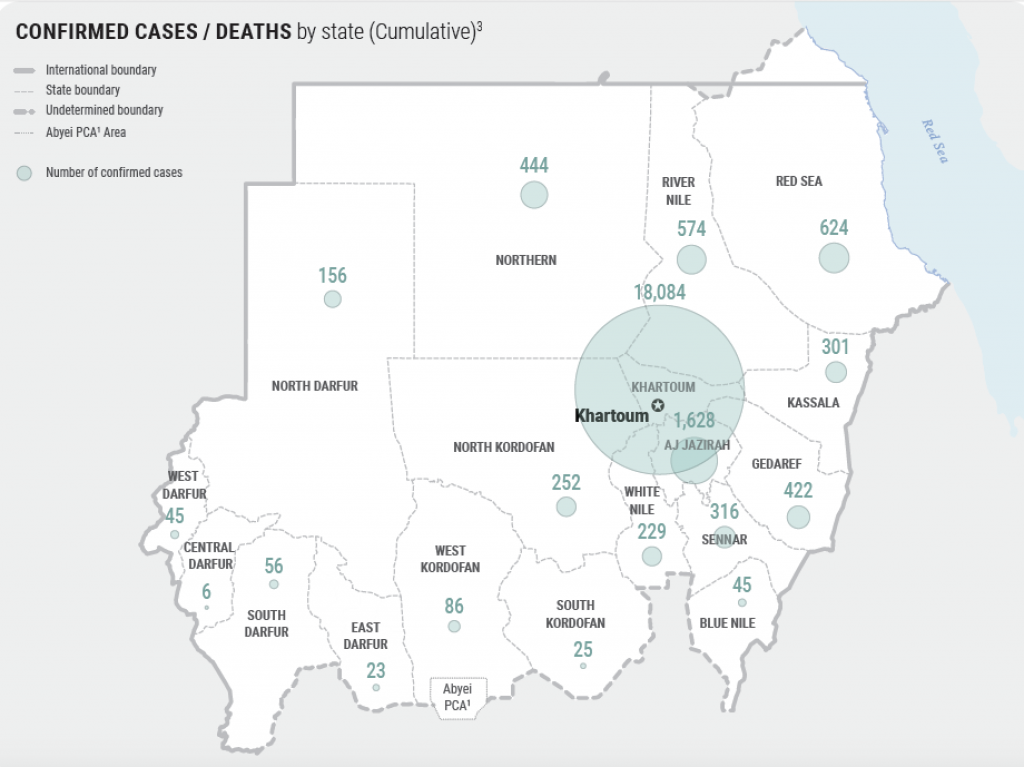
While Khartoum has the highest Covid-19 infection rate – representing 75% of all recorded cases, according to the national health ministry, it is certainly not the only area affected by the pandemic. According to a press statement on 2 January by the Director-General of the al-Gezira State Health Ministry, Ahmed al-Mustafa, the state has 600 cases of Covid-19 infection and over 100 virus-related deaths. In late December, the state’s Health Emergency Committee took drastic measures to curb the spread of the virus, everything from closing the market, postponing the school year, shortening prayers and reducing passengers on public transport. The head of the committee and state governor, Abdullah Idris al-Kinin, described the state’s health conditions as “dangerous and liable to explode”.
State officials are still perplexed as to why al-Gezira is experiencing this recent influx of Covid-19 cases, but acknowledge the lack of equipment and facilities to tackle the problem are certainly contributing factors. “This morning we transported a dead body from the isolation centre to the Wad Medani cemetery via a rickshaw (a public, three-wheeled motorcycle taxi),” said health-volunteer Orabi Al-Nour.

Other parts of the country, such as the restive western Darfur region, are also facing a dearth of medical supplies, health personnel and facilities to contend with the pandemic. According to South Darfur State’s Director of Epidemiology and Disease Control at the state’s health ministry, Muzammil Adam, the second wave of the Covid-19 pandemic is much stronger than the previous wave, despite there being more information available than in the first period, pointing out the lack of equipment and medical personnel in the state. “The capacity of the only isolation centre in Nyala (the state capital and Sudan’s second-largest city) is very weak compared to the size of the population,” Adam said. The centre provides only 20 beds and six ventilators, he added, for a city population of roughly one million. Many medical personnel are also unwilling to work in the isolation centre due to the poor incentives and lack of protective equipment, he added.
Employees of South Darfur’s Emergency and Epidemic Control Department in Nyala stopped working in December to protest a lack of payment. The funds, according to the former Director-General of the state health ministry, Muhammed Idris, meant for the health employees were already distributed in the first wave of the pandemic. Representing the only laboratory in Darfur to examine coronavirus patients, the closure poses a serious setback to state efforts to contain the virus, says Rehab Alqam, Director-General to South Darfur State Health Ministry. The state has witnessed an influx of travellers from the road and via Nyala Airport, Alqam added, where no initial examinations for the virus took place. The Director-General of West Darfur State Health Ministry, Muhammed Yahya said the suspension of the testing laboratory in Nyala also impedes their work to quell the virus since West Darfur State has no testing facilities. “When Nyala laboratory stops, we have to send samples to Khartoum, which causes serious delays,” the director-general told Ayin.
But even prior to the Covid-19 pandemic, South Darfur State faced severe shortages of medical equipment and personnel. According to Dr Ammar Ahmed, a member of the state’s Central Doctors Committee, the number of doctors in South Darfur State is 254 while the state’s population exceeds 3 million people. “Leave alone the coronavirus,” says Aisha Ali, a mother who took her daughter to Nyala Hospital last November. “We find it even difficult to treat malaria. If you do not have enough coins to buy medicine, death becomes a normal reality here.”

A lockdown no one can afford
Some states have taken stricter measures than others to curb the spread of the virus –including states in Darfur—but a nationwide lockdown will not be revived as during the first wave of the pandemic, according to state actors. A source from the Federal Ministry of Health who is not authorised to speak to the media told Ayin that the new administration is trying its best to differentiate itself from the previous administration under former minister Akram Ali Al-Tom. The current minister, according to the source, fears his predecessor’s lockdown cost Sudan too much and wishes to separate himself from these past measures.
While a total lockdown may prove the safest solution to subdue the second wave of the virus, few can afford such stark measures. A survey conducted last year by the Sudan Central Bureau of Statistics and World Bank to measure Covid-19’s socio-economic impact on Sudanese households found that 20% of households could not afford to buy basic food staples such as bread and milk. A quarter of those surveyed who required medical assistance could not access it and 27% could not access or afford the medicine they needed.
 The Vaccine
The Vaccine
With little chance of another lockdown and limited medical support to contend with the pandemic, most Sudanese are placing their hopes in the vaccine coming to Sudan. Under the Kovacs initiative, a system designed to allow the middle to lower-income countries to access the vaccines, Sudan is expected to receive 8.4 doses of the vaccine in April, covering roughly a fifth of the population. The government will have to find alternatives to cover the remaining population through bilateral agreements with donor countries, says Dr Magdy Sabah Al-Zein, a professor at Ahfad University and founder of the Vaccination Initiative Website. According to Dr Sabah, at least 75% of the population must be vaccinated to rid the country of the pandemic.
Even if Sudan receives the vaccination on time despite the huge global demand, Dr Sabah says, distributing the vaccines across the country will be very challenging. Some of the vaccines, for instance, require cold temperatures to remain effective – this will prove difficult given the country’s searing heat in April and May, not to mention the repeated power cuts compromising the ability to keep these vaccines refrigerated. Once distributed, there remains another challenge seen all over the world: people who distrust vaccines. “We, in the vaccination initiative spotted a lot of rumours and misinformation about Covid-19 and the vaccines,” Dr Sabah told Ayin. Dr Sabah is coordinating with the ministry of health to provide the correct information about the vaccines and dispel some of the dangerous rumours, largely spread via social media.
While most health professionals paint a bleak picture of the country’s meagre response to the pandemic, there are some positive signs. Hamza Awadalla, an epidemiologist and community medicine specialist, said the current administration is finally addressing the health system in Sudan, an area ignored by the former government for decades. The 2020 annual budget for health, for instance, represented a nearly nine-fold increase to past federal health expenditure under former dictator Omar al-Bashir. “If nothing else, this pandemic has helped expose a major crisis in Sudan’s health system,” Awadalla said, “maybe now we can finally get the attention and support we need.”














